Chemotherapy in Breast Cancer
- What is Chemotherapy?
- How is it administered?
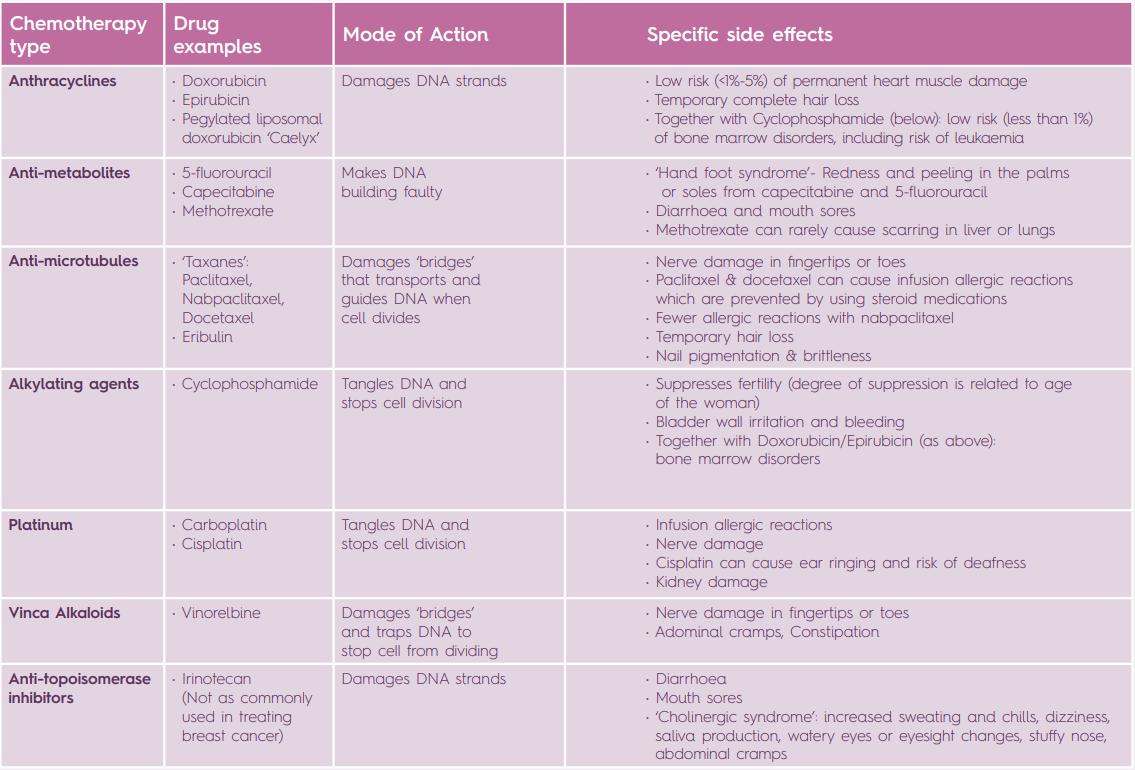
- Chemotherapy drugs being used to treat breast cancer
- Side Effects
- How to manage certain specific side effects?
Chemotherapy is the term used for drugs used to treat cancer. It generally stops cancer cells from dividing inside your body, leading to the cancer cell’s death. Cancer cells are particularly sensitive to chemotherapy due to their ability to grow much faster than normal healthy cells. Unfortunately, some normal healthy cells can still be affected by chemotherapy but to a much lesser degree and the normal cells usually recover once chemotherapy has been finished.
Normal healthy cells that are most affected by chemotherapy are those that naturally replenish themselves in your body. These include cells lining your gut, hair, skin and bone marrow (this is the place where your blood cells are made). This explains why the common chemotherapy side effects include nausea, vomiting, diarrhoea, hair loss, low white cell count (which can increase risk of infection) and low platelet count (which can increase bruising).
The current chemotherapy drugs that are given to women were carefully selected and approved by the Australian government’s Department of Health after being tested through many international drug trials involving hundreds to thousands of women. These drug studies were carried out to find the best treatments that would work to treat breast cancer, understand the chemotherapy treatments’ correct dosing level and their related chances of side effects.
The chemotherapy drugs that you will be prescribed, either alone or in combination, will only be used when there is proven benefit shown and when all possible side effects are known so that the right drug for the right patient can be recommended.
Chemotherapy is most often given through a drip into your arm vein. The treatment can be given through a removable plastic tube, also known as a cannula. This is inserted by trained nurses and removed after chemotherapy is completed.
Other ways of accessing your veins would be through a ‘PICC line’ or a ‘Port’. A ‘PICC line’ is usually inserted under ultrasound guidance in the x-ray department and can be left in your arm for weeks before it must be changed or removed. The plastic tubing can be seen outside your skin where it is inserted and needs to be dressed or taped onto the upper arm. A PICC line needs to be ‘flushed’ by a nurse once a week.
A ‘Port’ (a small rounded plastic chamber connected to a tubing) is usually inserted in the operating theatre by a surgeon and sits under the skin below the clavicle (collar bone). The Port is fully enclosed under your skin, so once healed, there is no limitation to swimming or exercise. It can remain with the patient for life or be removed at a much later date similarly in theatre.
Chemotherapy treatments may include one or more drugs given together at one sitting, with one bag of drug being infused after another. They are usually given for one or more days in a row, with a planned break from the chemotherapy drugs. This is termed a ‘cycle of treatment’.
The number of cycles that you will need, and the number of days in a cycle will be explained to you at the time the chemotherapy treatment is recommended by your oncologist.
Some chemotherapy treatments are given orally in tablet form. Examples include capecitabine and vinorelbine. It is important to understand that although these therapies are in a tablet form, they are no less potent than intravenous administration and still must be taken with care, by following the instructions of your oncologist or breast care nurse.
Early Breast Cancer (cancer confined to the breast and nearby lymph nodes)
Compared to many decades ago, the rate of curing breast cancer has significantly increased with the use of chemotherapy (as well as hormonal and biological drugs – see relevant BCRC-WA pamphlet for information on these drugs). Depending on the stage and type of early breast cancer that you have, chemotherapy is given either before or after surgery to shrink the cancer and reduce the risk of breast cancer returning in the body.
Chemotherapy when given before surgery is called ‘neoadjuvant therapy’ and has been shown in large clinical trials to be able to shrink large breast cancers to allow your breast surgeon to successfully remove the cancer either with a lumpectomy or a mastectomy.
In the past several years, giving neoadjuvant chemotherapy for particular types of breast cancers, can also allow choosing the best drug therapy after surgery, when the pathologist is able to fully examine the breast and lymph nodes.
Treatment after surgery is called ‘adjuvant’ treatment and aims to mop up and kill any potential floating cancer cells inside the body and prevent them from seeding into other organs in the future, thus preventing a recurrence of the original breast cancer.
Chemotherapy dose is calculated based on your own individual height and weight. It is important for chemotherapy to be given on time and at the correct dose. Research has shown that patients having chemotherapy at the right dose and number of cycles will have the best chance of reducing a return of the breast cancer.
It is therefore important that you inform your oncologist and breast cancer nurse of what side effects you have, so you are well supported during chemotherapy and can complete the full intended chemotherapy doses.
Metastatic or Advanced breast cancer (cancer has travelled into other organs outside the breast)
Breast cancer is classed as ‘metastatic’ or ‘stage 4’ when it has spread to or returned in an organ or tissue outside of the breast or local lymph nodes. This stage of breast cancer is usually regarded as incurable.
The role of chemotherapy in this setting is to kill as many breast cancer cells as possible, or to slow growth of those cells. Achieving this aim will lead to lessening of symptoms and prolongation of life. Chemotherapy dosing in this setting is tailored towards improving patient’s quality of life and minimizing side effects. You may still need additional supportive medications to manage any side effects.
General side effects
General chemotherapy side effects can include the following:
Nausea: Nowadays there are very effective drugs for nausea and majority of patients will experience no or mild nausea.
Diarrhoea: This can be managed with anti-diarrhoea medications including loperamide.
Mouth or Oesophagus (‘food pipe’) inflammation/ulcers: This can be managed with good oral care including moistening mouthwashes, salt and bicarbonate washes, topical steroid treatment directly on the ulcer (Kenalog ointment) and anaesthetic mouthwash – which needs to be prescribed.
Low white cell count (neutropaenia): White cells are cells that fight bacterial infections. The time it takes for a drop in the white cell count depends on which chemotherapy drug you are having. Usually, the lowered white cell counts only lasts for 1-4 days. The white cells will always recover with time. It is important to monitor for signs of infection such as fever (temperature >38C degrees), cold shivers or shakes, burning urine, redness at a site of a cannula insertion, cough or viral symptoms. Your body will not be able to fight infection whilst white cells are low and you may need oral antibiotics or antibiotics through a drip. Please contact your oncology team if you are unwell or have signs of infection during chemotherapy. Medications can be used to reduce the risk of infection whilst on chemotherapy. These ‘immune booster drugs’ include ‘Filgrastim’ or ‘Pegfilgrastim’, which is an injection administered under the tummy skin 24 hours after the dose of chemotherapy. Your oncologist will advise you whether you need to have the immune booster.
Low platelet count (thrombocytopaenia): Platelets are cells that help to stop bleeding. Some patients may bleed easier from places such as the gums or skin (if cut or damaged). The platelets will recover with time.
Hair loss: This happens whilst on certain chemotherapy and hair naturally grows back when chemotherapy stops. Cold cap therapy can reduce the chances of this. This can be discussed with your oncologist.
Fatigue: Whilst common, this can be managed by continuing gentle exercise and regular activity during chemotherapy and avoiding weight gain. Excessive resting can worsen fatigue and increase the risk of infections and blood clots. It is better to remain active during the day when on chemotherapy.
Psychological side effects: Some patients may experience reduced mental alertness, known as ‘brain fog’ or ‘chemo fog’.
Early menopause and loss of fertility: Patients who are still having periods may have temporary or permanent ‘early’ menopause as a result of chemotherapy. This can impact on fertility and you should discuss this with your oncologist prior to commencing chemotherapy treatment. There are options to maintain fertility such as egg collection and storage or a hormone injection to ‘switch off’ the ovaries prior to starting and during chemotherapy. You may need to be referred to a fertility specialist.
Psychosocial impact: Being on chemotherapy can impact on your ability to work, look after – or interact with your family or even your own self-care. It is important to involve your family and/or friends in your care so you can have as much support as possible. There is additional support available from the Perth Breast Cancer Institute and Hollywood Private Hospital including psychologist, physiotherapists and social workers, so please let your oncologist or breast care nurse know if you are having any difficulties in this aspect of your life.
Heart muscle damage: Anthracycline chemotherapies (Doxorubicin or Epirubicin) can cause permanent heart muscle damage leading to poor pumping function in a small percentage of patients (approximately <1%-5% of patients) many years after treatment.
The risk is dependent on higher doses, whether you need anti-HER2 drug therapy and the presence of heart risk factors before your breast cancer diagnosis. Safe doses of anthracyclines are used in breast cancer. Presence of other risk factors for heart disease such as age, smoking history, diabetes or hypertension can increase risk of further damage to the heart.
A heart scan (either echocardiogram or gated heart scan) is usually requested prior to starting these chemotherapies. You will be asked to monitor for any concerning symptoms (such as shortness of breath, leg swelling, breathlessness when lying flat) as early treatment can improve heart function.
Regular heart health checks, exercise and maintaining a healthy diet, safe blood cholesterol and sugar levels and blood pressure will help to reduce the risk of this side effect.
Hand-foot syndrome: This can frequently occur with capecitabine and 5-fluorouracil and presents with redness and pain to the palms and soles; more serious levels include skin blistering, peeling and fissuring. The nails can also be involved.
Management includes skin care with moisturizers, keeping away from prolonged water exposure (such as dishwashing), wound care and topical steroids. Sometime the dose is reduced or interrupted at the advice of your oncologist.
Nail changes: Some chemotherapy drugs can cause nail changes, especially Taxanes – such as paclitaxel and docetaxel – leading to dark pigmentation of the nails, splitting and sometimes loss of the nail.
Although there is no specific treatment for this, you can focus on avoiding infections, particularly fungal infections, by using topical antiseptics or anti-fungal creams if required.
Infusion allergic reactions: Taxanes (paclitaxeland docetaxel) are the most common drugs which cause allergic reactions whilst the drugs are being given. Symptoms include heart racing, flushing, itching, shortness of breath, back pain, throat tightening and high blood pressure during the infusion. This is usually short lived and stops once the chemotherapy infusion is temporarily stopped.
As it usually is not a true ‘allergic’ reaction, infusion reactions can be managed with steroids and antihistamines given prior to the chemotherapy. Once the reaction settles, the chemotherapy drugs can then be given again at a slower infusion rate.
Nerve damage: Tingling, numbness or pain in the extremities (toes and fingertips and sometimes lips) and can occur with certain chemotherapies as a result of nerve damage. The degree of nerve damage and related symptoms increases with more doses of chemotherapy.
Nevertheless, most cases of nerve damage improve or completely resolve with time. In a minority of cases, there may be persistent nerve symptoms.
Apart from managing chemotherapy doses to reduce this side effect, painkillers which target nerve pain (such as Gabapentin or Pregabalin) can be given as pain relief. Please inform your cancer team if you start experiencing any possible nerve damage symptoms.

Our full range of Resources
Breast Cancer Research Center – WA aims to support and educate breast cancer patients. For a specific pamphlet, ask our staff at your next appointment or download it from our website.
